While In Coma, My Husband and Lover Planned My Burial, Until The Nurse Said ‘She’s Back’ Then | HO

When the monitor beside Emily Carter’s hospital bed flickered, and the nurse registered the faintest tremor in the patient’s right hand, the change was almost imperceptible. It was the kind of movement that in any other circumstance could have been dismissed as reflex or electrical misfiring. But here, in a quiet medical ward where Emily had lain in a coma for weeks following a single-car accident on a rain-slicked suburban road, the sign carried weight.
It marked the moment when a story that had, until then, been quietly tragic took a darker, more unsettling turn.
Because in the same room where a wife hovered between consciousness and oblivion, her husband and the woman he was secretly involved with had stood over her bed and discussed her funeral.
And, critically, someone heard.
This is not simply a story about a medical recovery. It is a story about power, control, the uncomfortable gray spaces in health care decision-making, and what happens when a patient becomes unable to speak for herself—while those who do the speaking may not have her survival foremost in mind.
A Marriage That Seemed Solid — From a Distance
Until the accident, Emily’s life looked, from the outside, reassuringly ordinary. Thirty-two years old, college-educated, steady in her career, she had married Daniel Carter, a charismatic professional who presented himself as attentive, generous, and publicly devoted. Family members say Emily had an instinct toward loyalty. She was the sort of person who remembered birthdays, who volunteered to drive friends to appointments, who tried to resolve tension quietly rather than escalate it.
This disposition, those who later reviewed the case say, may also have made her particularly vulnerable to coercive dynamics masked as care.
Daniel was, by all accounts, a skilled communicator. He praised his wife in public. He sent flowers. He routinely referred to her as “the love of my life,” a phrase that echoed through the ward during her hospitalization. Yet, as investigators would later establish, he had also been conducting an affair with Lauren Price, a colleague who appeared at the hospital under the polite pretense of being a “family friend.”
What neither expected was that a staff member would overhear them discussing whether it might be easier if Emily never woke up.
The Accident
The crash itself, while severe, raised no immediate suspicion.
It was raining. The road curved. The vehicle collided with a barrier. Emergency responders arrived quickly. There were no other cars involved. Toxicology screens were negative. The working assumption was tragic misfortune.
Emily arrived at the hospital unconscious with significant head trauma, medically stabilized but unresponsive. After neurological consultation, physicians recommended close monitoring and supportive care. For families, such prognoses are uniquely difficult: modern medicine can sustain organ function while the brain’s future remains uncertain. Weeks can pass without meaningful change.
Into this uncertainty stepped Daniel, who signed forms, spoke with physicians, and updated relatives. He seemed, nurses recalled, composed. Helpful. Cooperative.
He also appeared frequently. And he was rarely alone.
A Nurse Hears Something She Cannot Ignore
Hospitals are busy places where overheard grief is common. Health-care workers encounter families in the rawest moments of fear and exhaustion. But what Nurse Karen O’Neal heard one afternoon, she later told colleagues, was different.
Standing just outside Emily’s door, chart in hand, she paused when Daniel’s voice sharpened to a whisper:
“Let her die. She’s useless now. Dead weight.”
The words were not spoken in panic. They were measured. A second voice—female, controlled, familiar to staff by now—answered with quiet, unsettling practicality.
The nurse did not move immediately. She listened as the conversation turned to insurance payouts, revised paperwork, and the blunt logistics of what would follow if Emily were declared beyond recovery.
Nurses are trained observers. They are also bound by policies, hierarchies, and the risk of misinterpretation. For a time, Karen did what the system so often forces professionals to do: she watched closely, documented meticulously, and waited for facts.
Then the signs began to multiply.
Discrepancies and Pressure
In the days that followed, Daniel returned frequently, often with Lauren near the hallway, lingering just beyond the threshold. He asked pointed questions about life-support directives. He referenced an alleged “updated living will” that, when reviewed, contained signature irregularities. He pressed physicians to consider withdrawal of care, despite neurological findings that did not support such action.
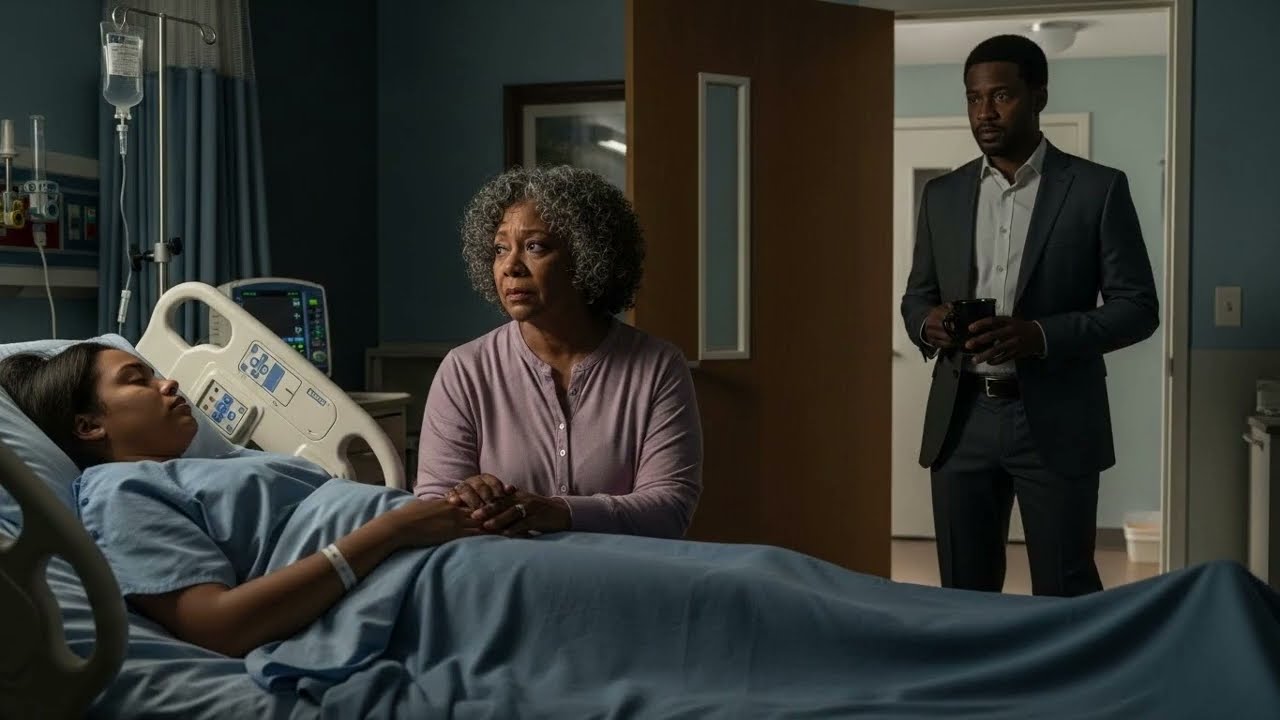
When confronted with questions from Emily’s mother, Carol, Daniel deflected with plausibly gentle explanations. He portrayed himself as a pragmatic husband facing an impossible reality. Carol, increasingly uneasy, noticed his restlessness—the constant checking of text messages, the mounting distance in tone.
Several nurses observed similar patterns, though most stopped short of formal complaint. In health care, intuition alone is not actionable. Documentation is. And so charts accumulated notes regarding visits, demeanor, and remarks.
One constant remained: Karen’s vigilance.
The First Sign of Something Changing
Then came the morning when a finger moved.
Karen had entered Emily’s room with linens, prepared for another routine round of care. Sunlight filtered through the window blinds. The day felt unremarkable.
Emily’s right index finger twitched—once, then again.
Karen froze. The muscle memory of a career responded first: she checked reflexes, verified readings, paged a physician. Dr. Foley, the attending, confirmed the movement and ordered further neurological testing.
“This could be the first sign of recovery,” he told the staff, cautious but hopeful.
Daniel entered mid-evaluation. The nurse expected relief. What she saw instead was something closer to alarm.
It was a fleeting expression—there and then gone—but unmistakable to someone who had been watching for weeks.
A Husband’s Panic
According to interviews and contemporaneous notes, Daniel asked a string of practical questions. Could patients sometimes remember conversations that occurred during comas? Could emerging awareness include recollections? How reliable were such memories?
These inquiries, while not inherently suspicious, gained significance in light of the earlier overheard conversations. Karen’s professional concern sharpened into protective watchfulness.
Policies required her to maintain composure and fairness. But privately, the nurse began to worry—not only about Emily’s prognosis, but about her safety if she regained consciousness.
Her fear was not theoretical.
Because shortly after the doctor left the room that day, Daniel closed the door.
And for the first time since the accident, the veneer of the “devoted husband” appeared to fracture.
Control Without Witnesses
What occurred during that closed-door interval would later be reconstructed from a combination of internal audio monitoring, staff observations, and, eventually, law-enforcement review.
Daniel spoke calmly to his unconscious wife. He told her, according to recordings, that waking up would “ruin everything.” He expressed fear—less for her health than for the consequences to his own life should she speak.
This was the pattern prosecutors would later call ownership disguised as concern.
When staff returned, Daniel’s demeanor reset to its familiar setting. He thanked nurses. He referenced prayers. He positioned himself as the anchor of a family in pain.
But the gap between the public and private husband was widening. And the person who noticed most sharply was the nurse whose instinct had already been piqued.
Pressure Expands Beyond the Hospital Room
Meanwhile, Emily’s mother, Carol, continued to sense distance and contradiction.
She noticed a woman—Lauren—appearing often on the unit. She noticed tension when she confronted Daniel about it. She received emails, allegedly from Emily, describing estrangement from her family and hints of divorce.
Those emails would later be identified as forgeries.
“Control rarely begins with dramatic gestures,” said a clinical social worker familiar with the case. “It begins with subtle isolation—gradually removing support so that the victim’s perspective can be rewritten.”
In this instance, the rewriting extended beyond Emily to those around her: recasting a mother as “emotional,” a nurse as “interfering,” a wife as “difficult” or “unrealistic.”
The result was a shifting perception map in which Daniel remained the steady center.
Until the day Emily’s body decided otherwise.
“She’s Back”
Recovery from a coma is not cinematic. There is no sudden gasp, no immediate clarity. It is incremental: fingers first, then facial muscles, then brief flickers of eye movement.
Emily’s return followed this pattern.
Karen observed another deliberate finger movement. Then the faintest tremble of eyelids. Over hours, then days, Emily began to surface from the fog—hovering between awareness and exhaustion, her body a step behind her mind.
When her eyes finally opened for more than a moment, the nurse leaned forward, speaking gently, grounding her in the new reality.
“You’re safe,” she said. “We’re here.”
But safety, Emily would soon learn, was still fragile.
Because the first person to enter after she stabilized was Daniel.
He saw her eyes open. He froze.
And she—weak, barely able to form sound—managed one word:
“Why?”
It was less accusation than plea. But to a man who, according to investigators, had built a web of deceit around her presumed silence, the syllable landed like a threat.
A System Catches Up
From that point, the pace shifted.
Hospital risk management and legal counsel reviewed audio surveillance, as is standard in certain high-risk care contexts. Physicians re-evaluated sedative protocols. The nursing staff escalated concerns to supervisors. Security staff began to monitor access.
Within days, law enforcement was quietly notified.
The recordings that emerged painted a picture prosecutors later described as “chilling in its composure.” In the room of a defenseless woman, her husband and his lover had planned her funeral, discussed inheritance, and debated timing—all while she remained alive.
Worse still, recordings and witness statements suggested that braking issues preceding the accident were not entirely accidental.
By the time detectives visited Daniel, the narrative had shifted decisively.
A Patient Finds Her Voice
Emily’s physical recovery was slow but measurable. Speech returned in fragments. Therapists encouraged tiny movements, then steps. Amid the work of rehabilitation, she carried the heavier burden of memory—piecing together shards of the time before the crash, the arguments, the isolation, the subtle rewriting of reality that had crept into daily life.
She also processed something else: the discipline of composure shown by medical staff who believed her when evidence emerged, and who acted within the structure of a system that does not move quickly unless it must.
In interviews, hospital administrators would later emphasize the difficulty of such situations. Health-care workers cannot accuse without proof. But they are obligated to report patterns that suggest risk.
Here, a nurse’s early instincts proved prescient.
A Broader Question
Cases like Emily’s force an uncomfortable reckoning—not only with individual wrongdoing, but with how dependent we become when unconscious, and how much power rests in the hands of those designated as our decision-makers.
What safeguards exist when those entrusted do not act in our interest?
How early can institutions detect the difference between grief and manipulation?
And what does it mean, ethically and practically, when victims of domestic coercion also become patients unable to speak?
These questions now animate policy discussions among clinicians and lawmakers alike, particularly around recognizing coercive control as a form of violence before it escalates to physical harm.
For Emily, the debate is not abstract.
It was, quite literally, a matter of survival.

When physicians confirmed that Emily Carter was emerging from the coma, the hospital moved swiftly but quietly. A security officer began logging visitors. Nurses updated records with precision. And a detective from the major-crimes unit arrived in an unmarked sedan, carrying a small leather notebook and an air of practiced calm.
The notebook would eventually fill with the slow, disciplined accumulation of detail that criminal prosecutions require. Audio files. Visitor logs. Email metadata. Insurance documents. Mechanics’ reports. Subtle shifts in tone recalled by nurses over coffee breaks between shifts.
But on that first day, the detective focused on something deceptively simple:
Who had power while Emily did not.
XXVI. The Investigation Becomes Formal
It began as a safeguarding inquiry — the sort of quiet internal review institutions initiate when patterns of concern appear. No accusations. No headlines. Just questions.
Soon, however, the inquiry intersected with emerging medical evidence: the car involved in Emily’s “accident” showed signs of prior tampering — specifically with brake lines and components ordinarily inaccessible without deliberate effort.
Police obtained a warrant.
Mechanical examination corroborated the suspicion.
The crash that placed Emily in a coma had not been wholly incidental.
It now existed within a widening legal frame.
The investigation transitioned from protective to criminal.
XXVII. Two Parallel Realities
Inside the hospital, Emily’s world expanded inch by inch — first eye contact, then a nod, then whispered syllables. Speech therapy retrained muscles. Occupational therapy reintroduced movement. The mundane, exhausting victories of recovery accumulated.
Outside those walls, detectives mapped an entirely different trajectory — a relationship that had been deteriorating well before the crash.
Phone records revealed the volume of messages between Daniel Carter and Lauren Price spiking weeks prior. Email drafts — recovered even after deletion — contained discussions of insurance clauses, asset division, and travel plans inconsistent with the public picture of a grieving spouse.
Investigators traced visits by Lauren to the ward, often scheduled when Emily’s mother was absent. Nurses noted a visible effort between the pair to minimize the presence of witnesses during conversations.
Patterns emerged.
Paperwork shifted.
The timing aligned disturbingly with the crash.
None of this, taken alone, proved guilt.
Together, it formed context.
XXVIII. The Ethical Fault Line in Health Care
Hospitals operate at the intersection of privacy and protection. Patient autonomy is sacrosanct. Families are encouraged to participate in decisions. Yet when autonomy disappears — as in coma cases — the system must rely on proxies and legal designations.
Those proxies can be benevolent.
They can also, as this case revealed, be dangerous.
Clinical staff described the tension as a “balance beam over concrete.” Move too quickly toward accusation, and a family is wrongly harmed. Move too slowly, and a patient is left unprotected.
In Emily’s case, nurses did what training and law require:
They observed, documented, escalated, and waited until documentation rose to the level of evidence.
Without that chain, the criminal case might not have existed at all.
XXIX. The Arrests
Three weeks after Emily first opened her eyes, officers executed simultaneous warrants.
Daniel Carter was taken into custody at his workplace — a glass-and-steel office tower downtown. Coworkers later recalled his surprise as “muted, like he’d been expecting something, just not today.”
Lauren Price was arrested later that afternoon.
Both were charged with multiple felonies including attempted murder, conspiracy, insurance fraud, and evidence tampering.
Defense statements emphasized presumption of innocence and warned against “trial by rumor.” They argued that the overheard hospital conversations were expressions of grief mistranslated by stress, that brake issues could have been mechanical failure, that insurance discussions were “ordinary and prudent planning.”
Prosecutors countered with chronology.
Words are fluid.
Timelines are not.
XXX. A Patient Becomes a Witness
Emily, still in rehabilitation, now faced the dual burden of recovery and cooperation with law enforcement.
Her statements were taken with extraordinary care. A trauma-informed interviewer and psychologist sat in. Sessions were brief, structured, and optional. Investigators understood that consciousness returns in fragments and that memory formed around trauma can be both vivid and incomplete.
She remembered tension.
Arguments.
Financial pressure that seemed to intensify just before the crash.
She remembered Lauren’s presence in the weeks leading up to it — though at the time, she believed the colleague’s visits were incidental.
Most of all, she remembered the emotional drift — “as though my life was being narrated to me instead of lived,” she would later describe.
Her testimony did not stand alone.
But it corroborated.
And in criminal law, corroboration matters.
XXXI. The Courtroom as Mirror
Trials are rarely cinematic. They are procedural, relentless, governed by rules of evidence and the dry choreography of objection and reply. Yet in this courtroom, emotion seeped through the seams.
Audio from the hospital played softly over the speaker system — voices devoid of panic, discussing burial arrangements while a woman’s heart monitor beeped steadily beside them.
Jury members took notes.
So did journalists.
So did Emily’s mother.
Mechanics testified.
Insurance analysts testified.
Nurses testified — including Karen O’Neal, who spoke in the measured cadence of someone careful with both truth and responsibility.
The defense pressed hard.
Memory can be flawed.
Emotions can bias perception.
But the pattern — electronic records, physical evidence, recorded speech, and witness observations — resisted dismissal.
After weeks of testimony, the jury retired.
They returned the next afternoon.
Guilty.
XXXII. Sentencing and Silence
At sentencing, the judge spoke not of spectacle but of betrayal — not only of a spouse, but of the public trust that medical institutions place in family decision-makers.
“There are few moments in life where we are more vulnerable than when we are unconscious,” he said. “The law must be acute to the dangers that arise when that vulnerability is exploited.”
Daniel received a lengthy prison term.
Lauren, convicted on conspiracy-related counts, received a separate sentence.
There were no outbursts.
Just the heavy quiet of consequences settling into place.
XXXIII. The Long Work of Coming Back
After courtrooms emptied and headlines receded, Emily began the most difficult part of her story:
living forward.
Recovery was not linear.
Some days were composed.
Some were not.
She relearned balance and language. She built boundaries where once there had been unqualified trust. She surrounded herself with people whose presence came without condition or control.
And she confronted the disquieting truth that the person managing her care while she could not speak had viewed her life as negotiable.
Therapists call this a second injury — the emotional aftermath layered over physical trauma.
She chose, cautiously, to share portions of her experience with advocates who train hospital staff and community organizations about coercive control, medical decision-making, and early warning signs.
Her advocacy is consistent, not loud.
Measured.
Precise.
Like her.
XXXIV. Policy Ripples
The case prompted institutional review across the region.
Hospitals revisited protocols governing:
• Visitor limits in high-risk cases
• Documentation of concerning statements
• Ethical escalation channels for nurses and social workers
• The use of audio systems in intensive-care settings
• Collaboration guidelines with law enforcement
Legislators also began examining the legal authority of medical proxies — balancing the sanctity of family roles with guardrails for when third-party review becomes essential.
Advocates for domestic-violence survivors urged that coercive control — isolation, financial restriction, psychological manipulation — be taken seriously before violence escalates.
Emily’s case became a sobering example at conferences, trainings, and seminars.
Not for shock.
For instruction.
XXXV. The Nurse Who Listened
Throughout this process, one name surfaced again and again:
Karen O’Neal.
A veteran nurse with decades of quiet service, she did what her profession asks and society relies upon: noticed, documented, and spoke when the evidence required it.
She rejects language of heroism.
“I did my job,” she said once, when pressed.
Perhaps.
But her insistence on doing it thoroughly made all the difference.
XXXVI. What It Means to Be Safe
There is a photograph on Emily’s mantel now — not of the past, but of the present: parents, a sister, a small circle of friends gathered at a table strewn with ordinary Sunday clutter.
Coffee cups.
Folded newspapers.
A half-finished crossword.
She keeps it there, she has said, to remind herself that safety is not the absence of risk.
It is the presence of people who choose your life, unconditionally, without calculation.
XXXVII. The Question That Remains
Every investigation eventually reaches the same point — the fact pattern clarified, the verdict rendered, the legal narrative complete.
But completion is not the same as closure.
There remains the enduring question:
How do we protect those who cannot speak for themselves when danger comes disguised as devotion?
Hospitals will refine policies.
Courts will adjudicate cases.
Families will sit at kitchen tables and whisper concerns, uncertain when to act.
And somewhere, a nurse on a routine shift will pause outside a doorway — sensing that something is wrong — and will decide, painstakingly, whether the instinct in her chest warrants intervention.
In Emily’s case, it did.
And a woman who nearly vanished beneath the quiet efficiency of a funeral plan awakened instead to the sound of a nurse leaning close and saying softly:
“She’s back.”
News
3 Weeks After Their Wedding, He Sh0t his Wife 15 times for Getting Him the Wrong Christmas Gift | HO
3 Weeks After Their Wedding, He Sh0t his Wife 15 times for Getting Him the Wrong Christmas Gift | HO…
Hiker Vanished in Colorado — 5 Years Later, She Staggered Into a Hospital With a Shocking Truth | HO
Hiker Vanished in Colorado — 5 Years Later, She Staggered Into a Hospital With a Shocking Truth | HO On…
The Bank Called: ‘Your Husband Is Here With A Woman Who Looks Just Like You…’ | HO
The Bank Called: ‘Your Husband Is Here With A Woman Who Looks Just Like You…’ | HO At 2:47 p.m….
Teen K!ller LOSES It In Court After Learning She’s Never Going Home | HO
Teen K!ller LOSES It In Court After Learning She’s Never Going Home | HO In the final moments before the…
Mother Caught Cheating With Groom At Daughter’s Wedding – Ends In Bloody Murder | HO
Mother Caught Cheating With Groom At Daughter’s Wedding – Ends In Bloody Murder | HO On a warm evening in…
I Cared For My Paralyzed Husband For 5 Years. Then A Doctor Said ‘Call The Police.’ | HO!!
I Cared For My Paralyzed Husband For 5 Years. Then A Doctor Said ‘Call The Police.’ | HO!! The fluorescent…
End of content
No more pages to load